Empowering Women and Girls: Understanding and Managing Obstetric Antiphospholipid Syndrome (OAPS)
Obstetric Antiphospholipid Syndrome (OAPS) is often linked with recurrent miscarriage, but it can lead to various other pregnancy complications.
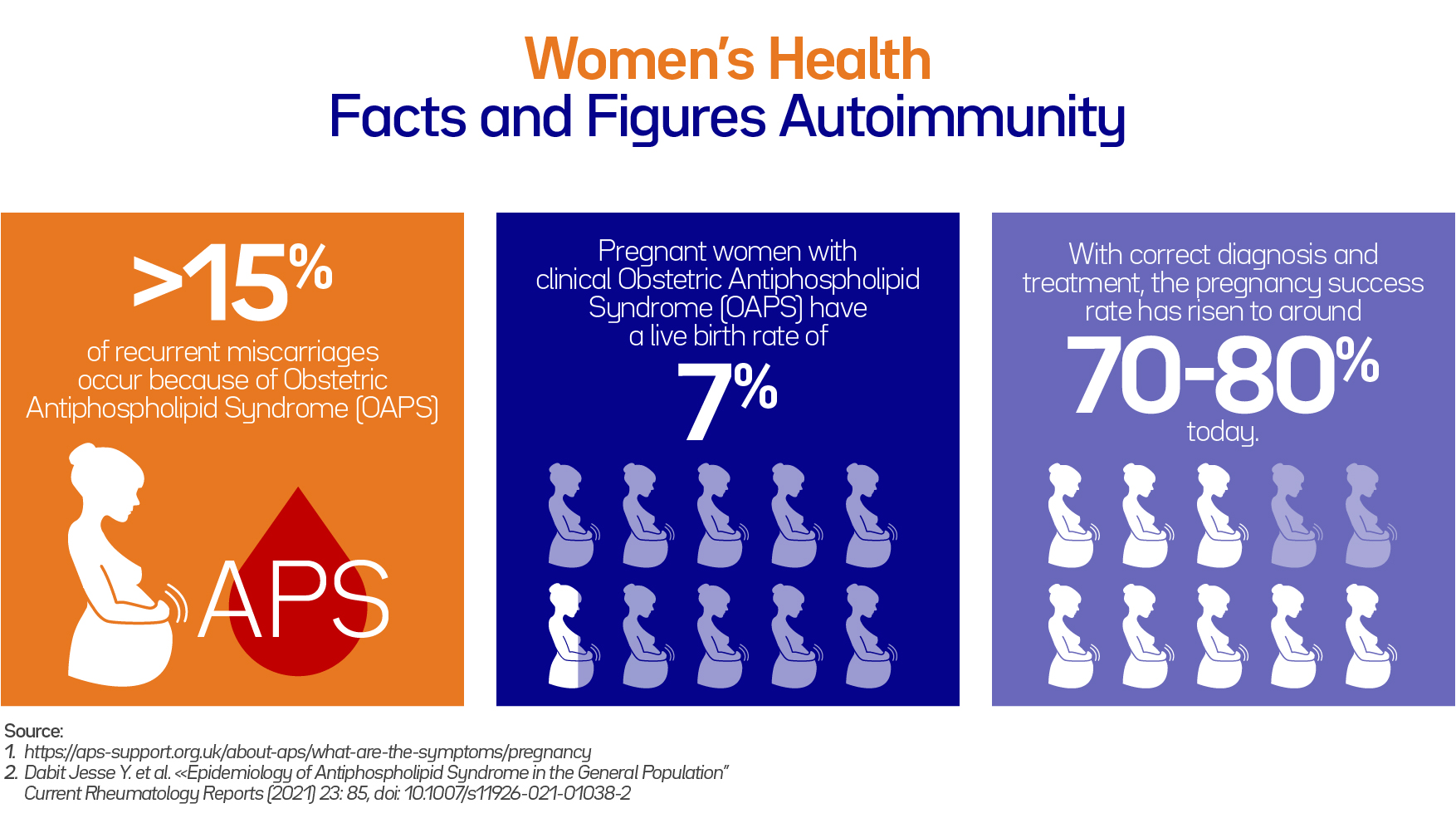
Recurrent miscarriage, defined as experiencing three or more consecutive miscarriages, affects approximately 1% of couples attempting to conceive. APS accounts for at least 15% of recurrent miscarriages and is now recognized as the most common treatable cause.
With proper diagnosis and treatment, the success rate of pregnancy has increased from 20% before 1990 to around 70-80% today. Given the high-risk nature of APS pregnancies, seeking care from a specialized or early pregnancy unit with experienced clinicians is advisable.
Treatment varies based on individual medical history, test results, and current conditions. Generally, women diagnosed with APS are recommended to take aspirin and heparin from a positive test until at least 34 weeks of gestation, following a discussion of potential benefits versus risks. This typically involves daily low-dose aspirin (75mg-150mg) and daily heparin injections. If a woman is already on warfarin for APS before becoming pregnant, transitioning to daily heparin injections, ideally before the embryo reaches six weeks, is necessary due to the potential harm of warfarin to the baby. While some women with APS may have successful pregnancies without treatment, pregnancy loss or complications often serve as the initial or sole indicator of the condition.
Pregnancies affected by APS can manifest in several ways:
Early Pregnancy Loss: Most miscarriages in women with APS occur within the first 13 weeks of pregnancy. Antiphospholipid antibodies (aPL) hinder proper embryo implantation in the womb and impede early fetal cell growth, contributing to early miscarriages. Late Pregnancy Loss: Losing a baby in the second and third trimesters (from 14 weeks until birth) is rare in most pregnancies but strongly associated with APS.
Late pregnancy losses often result from clots formed by aPL in the delicate veins of the placenta, leading to inadequate nutrient and oxygen supply to the baby.
Pre-eclampsia: Pre-eclampsia, affecting up to 10% of pregnancies, is twice as likely in women with APS and tends to be more severe. It is believed to result from inadequate blood supply to the placenta, potentially due to clotting caused by aPL. Pre-eclampsia poses risks to both mother and baby, necessitating careful monitoring and sometimes premature delivery.
Intrauterine Growth Restriction (IUGR): IUGR, affecting 10-30% of babies born to mothers with APS, refers to reduced fetal growth in the womb. Damage to the placenta by aPL can hinder normal fetal development, leading to smaller-than-average babies at birth. Doppler ultrasound scans are used to monitor fetal blood supply and guide decisions regarding delivery timing.
Overall, understanding the complexities of APS and its impact on pregnancy outcomes is crucial for effective management and improved maternal and fetal health.
To learn more about OAPS check out these two articles:
Taking Action: Steps for Awareness and Advocacy
1. Education and Advocacy
Raising awareness is fundamental to empowering women with Obstetric Antiphospholipid Syndrome (APS). It's crucial to educate women about the signs and implications of this condition during pregnancy. Advocacy efforts should push for better understanding and recognition of Obstetric APS in healthcare settings and communities.
2. Seeking Specialized Medical Advice
Encouraging women with Obstetric APS to seek specialized medical advice is paramount. Obstetricians with experience in managing high-risk pregnancies and APS should be consulted for proper diagnosis and management. Timely intervention can significantly improve pregnancy outcomes for women with Obstetric APS.
3. Support and Counselling
Access to support groups and counseling services is essential for women navigating Obstetric APS. These resources offer emotional support, coping strategies, and a platform for sharing experiences. Connecting with others facing similar challenges can alleviate anxiety and provide a sense of solidarity.
4. Research and Collaboration
Investing in research focused on Obstetric APS is critical for advancing knowledge and improving outcomes. Collaboration among healthcare professionals, researchers, and patient advocacy groups is key to driving progress in understanding and managing this complex condition. By supporting research initiatives and fostering collaboration, we can enhance care and support for women with Obstetric APS and their families.

